Category:Introduction to Public Health and basic concepts
Contents
Definition of public health
“… the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organisations, public and private, communities and individuals.". This definition is over one century old but remains valid, despite all societal changes. Public health is a field where many disciplines and many professional sectors collaborate.
Relevant disciplines and sectors within public health:
- epidemiology
- microbiology
- biostatistics
- health services
- environmental health
- community health
- behavioural health
- health economics
- informatics
- public health interventions
- public policy
Mortality statistics and health priorities
Which diseases are important for public health? Are they those that most people die from? In that case, we should concentrate on preventing/curing the main causes of death. Or....? There is always ‘a most common cause of death’ in the population. Take a look at this pie chart that represents the proportional distribution of mortality in a hypothetical population for 5 causes of death :
In the above case this is ‘disease A in red’. Yet imagine what happens when we successfully eliminate that disease...... then there will be another disease that will be the biggest:
This is easy to imagine when we consider that no man is immortal: “mortality in the EU is 100%”. This creates a fundamental question in public health: Which would we consider the best distribution of causes of death? or: How do we want to die?
Perhaps in all of human history, we are among the first generations that actually may have an active choice about the distribution of causes of death in society. In the EU, half of those who die are over 75-80 years old. Their causes of death will greatly influence mortality statistics. What role will this play for research, prevention, resources?
Measuring the health of the population. How can we measure ‘the health of the population’?
One indicator is the average life expectancy. Surely a population where people die before they are 40 can be considered less ‘healthy’ than one where most people reach 80? Perhaps, but the ‘average age’ is very much influenced by child mortality: if half of the children that are born die at birth and the rest lives exactly until 100 years, then the average life expectancy is 50 years.
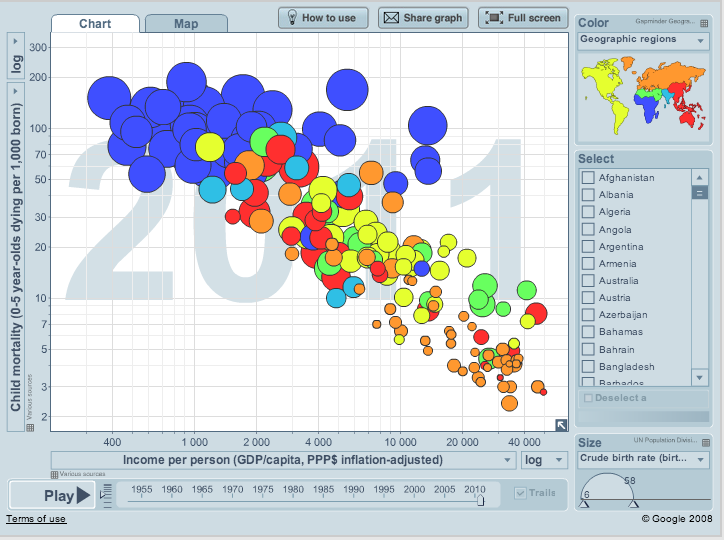
And it appears that child mortality (under 5 years old) is also a very good indicator of the population health.
(Image from the Gapminder)
However, if we all spend the years we live while suffering from chronic diseases, could we still call that ‘more healthy’?
If we want to correct for years spent with diseases, the indicator of DALY (disability adjusted life years) is often used. DALY’s are based on two things: (1) Life expectancy and (2) Number of years with less than full health.
But how do you measure disability?
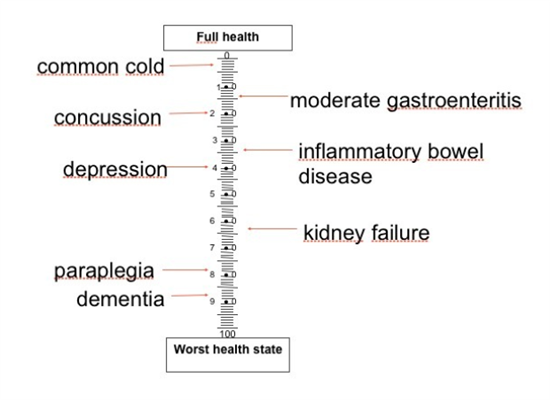
On a scale from 0 to 100, where 0=death and 100 is ‘total health’, how much are various ill healths? One way of finding out is to interview people, and ask them to indicate on that scale how they would feel if they had a common cold, or diarrhea, or when they lost an arm or a leg, or become paralyzed....
If you ask many people, the ‘average scale’ could look like the one above. It also appears that the resulting scales differ a lot between countries. By attaching a DALY value for each disease, and measuring how common this disease is in the population the actual burden of this disease can be assessed. A useful tool for public health (and sometimes quite surprising).
Some important Definitions
When reading general texts in public health, you will encounter certain epidemiological indicators often. Here is an overview of the most common ones, and their definition. Advanced readers may use the hyperlinks to read more detailed descriptions about these indicators.
- Incidence (or cumulative incidence): the number of new cases per population. Usually per 100.000. Outbreaks usually show a higher incidence: the incidence is then expressed per thousand or per hundred (%). In outbreaks, cumulative incidence is often called 'attack rate'.
- Incidence rate = number of new cases of the disease per population and per time unit (most often per year and per 100,000 people)
- ”The incidence rate of chlamydia in the EU is 175 per 100,000 per year”
- ”The incidence of vCJD in the EU is 1 or 2 cases per year.”
- Prevalence = proportion of the population that have the disease right now
- ”The prevalence of high blood pressure in US adults is around 30%”
- ”Tuberculosis is eliminated from a country when prevalence is less than 1 per million.” Morbidity = almost the same as prevalence
- Lethality = proportion of people who get a disease that will die from it (also called ’case fatality’)
- Mortality = number of deaths per population (most often per 100.000)
- Proportional mortality= of all people who died, what proportion have died from this disease
- Mortality of Infectious Diseases in the European Union is quite low, except pneumonia (several % of all deaths) and influenza (0 – several thousands of deaths). This picture is very different from the rest of the world: globally, around 62 million people die each year, 25% of them from infectious diseases.
Globally, relevant infectious diseases causing significant mortality are:
| Pneumonia | 4.2 |
|---|---|
| AIDS | 3 |
| Diarrhoea | 2 |
| Tuberculosis | 1.7 |
| Malaria | 1.4 |
| Measles | 0.2 |
Followed by neonatal tetanus, pertussis, meningitis, syphilis and hepatitis. Even though they seem an important public health problem globally, so why are they important to the EU? In the next paragraph on the origins of public health, we try to find the answer, which lies in the success of prevention.
Origins of Public Health:
Though history shows many descriptions of preventive advice from various medical scholars, and social response against serious outbreaks included quarantine, the concept of ‘population health’ probably took off with the sanitation movement in the second half of the 19th Century. This led to promotion of clean water, sewage works, better ventilation, more light in the houses and work places and in general cleanliness, personal and in home.
In addition, improvements such as Safety at work, Vaccines, Food control were developed: it is clear that most of these interventions were very much concentrated on infectious disease. Perhaps we can consider this as ‘classic public health’:
- Mainly controlling risk factors that people could not be expected to control themselves
- Promoting better education, better housing, etc.
- Aimed at very large population groups
- Often linked to socio-liberal political movements
‘Modern public health’ seems much more targeted at individual human behavior; something each of us should be able to influence:
- smoking
- eating
- drinking
- exercise
- sexual health
- tanning
Both the classic and the modern approach have in common that public health involves almost all areas of society and attempts to:
- Identify the main determinants of ill health
- science-based action to eliminate or prevent them
In our current EU Law, Public Health is now clearly mentioned and the Union has a mandate in that.
Maastricht Treaty, 1992, Article 129:
“The Community shall contribute towards ensuring a high level of human health protection .. Community action shall be directed towards the prevention of diseases... Health protection requirements shall form a constituent part of the Community's other policies.”
Societal changes that influence the infectious disease panorama
- increased international traffic (goods, people)
- ecological changes (global warming/extreme weather)
- new production methods (for food, mainly)
- microbial adaptation (= resistance)
- changing contact patterns (mega-cities, sexual contacts)
- societal breakdown (conflicts, recession)
With all the above, it may be clear that in the EU we have been successful in pushing infectious diseases back as a significant cause of mortality. However, we also see that around the world, there is still many infectious diseases that are ‘alive and kicking’. When we look at the factors behind our success, we notice that our ever changing society may open many future doors for infectious diseases to come back in.
Final remarks:
- The present 'victory' of the rich countries over the infectious diseases is fragile
- The way we live is as decisive for infections as characteristics of microbe or host
- There will be new ones........
References:
- Winslow, Charles-Edward Amory. "The Untilled Fields of Public Health",Science, 1920; 51(1306): 23–33.
- www.gapminder.org: for a fact based world view. Map on child mortality and country income, 2011 data
- the Maastricht Treaty on the European Union (1992)
- Lecture by Johan Giesecke in "ECDC Public Health 101 course", October 2013
FEM PAGE CONTRIBUTORS 2007
- Editor
- Arnold Bosman
Subcategories
This category has the following 5 subcategories, out of 5 total.