Threshold setting
Most of the tests used to help diagnose a disease or condition in a person are not based on dichotomous measurement (0-1). Test results frequently correspond to continuous variables (ex. glycemia expressed on mm/L, optical density, etc..). In such situations we use a cutoff value above which (or below which) the test is considered positive (or negative). The positioning of a cutoff value will always constitute a compromise between sensitivity (i.e. picking up everyone who has the condition) and specificity ( i.e. avoiding healthy people being labeled as positive for the test).
Reasons for setting the line towards high sensitivity:
- Serious disease with definitive treatment
- Risk of infectivity to others
- Subsequent diagnostic test cheap and low risk
Reasons for setting the line towards high specificity:
- Unpalatable treatment
- Costly, risky subsequent diagnostic test
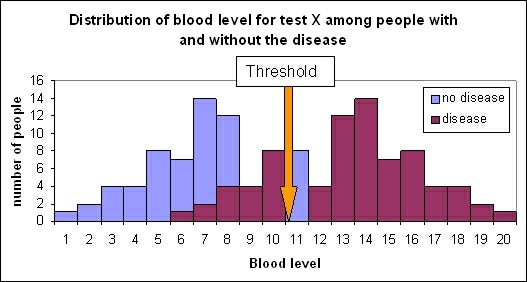
In a perfect ideal test the distribution of results for people with and without the disease would not overlap. In the situation described in Figure 1 a cutoff value of 11 would perfectly discriminate between the two distributions. This ideal situation is in fact very rare. More likely a situation occurs in which test values overlap between those without and with the disease (Figure 2).
Figure 1: Distribution of blood level for test X among people with and without the disease.
Figure 2: Distribution of blood level for test X among people with and without the disease.
Choosing an appropriate cutoff value in Figure 2 is more complicated. The decision what value to give the cutoff point depends on the condition tested for, availability and acceptability of treatment, risk for disease spread and the consequences of misclassification etc. It is important to fix a cutoff value which will correctly detect as many people with the disease or condition under study (true positives) and avoiding healthy people being labeled as positive for the test (false positives). Choosing a cutoff point is making a compromise between the sensitivity and the specificity of the test. The lower the cutoff value the higher the number of people correctly tested positive, but the higher as well the number of people incorrectly tested as positive. Alternatively the higher the threshold the higher the number of people correctly labeled as negative and the number of people incorrectly tested as negative. The choice of the threshold will either increase sensitivity or the specificity. It is a trade off. For example; If a disease is of particular public health concern the emphasis is on minimizing false negatives to avoid disease transmission (Ebola, Avian Influenza, etc.) [1].
References
1. Sheringham J, Kalim K, Crayford T. Mastering Public Health: A guide to examinations and revalidation. ISBN-13 978-1-85315-781-3.
FEM PAGE CONTRIBUTORS 2007
- Editor
- Maarten Hoek
- Original Authors
- Julia Fitzner
- Alain Moren
- Contributors
- Lisa Lazareck
- Maarten Hoek